The Global Clinical Risk Grouping Solutions Market is valued at USD 2.28 billion in 2026, and set to hit USD 4.19 billion by 2033, growing at 11.3% CAGR from 2026-2033.
The Global Clinical Risk Grouping Solutions Market comprises software and analytics platforms designed to stratify patient populations into risk categories based on clinical, demographic, and resource-related data. These solutions use predictive analytics, AI, machine learning, and big data to assess patient risk, support value-based care, optimize resource allocation, and improve clinical decision-making. They are widely adopted by hospitals, payers, ambulatory care centers, and long-term care facilities to enhance population health management, reduce healthcare costs, and improve patient outcomes by enabling precise identification of high-risk individuals and guiding preventive or personalized care strategies.
Key trends shaping the market include the increasing integration of AI and machine learning within risk stratification platforms, which enhances predictive accuracy and actionable insights. Healthcare providers are moving toward data-driven clinical decision-making, integrating electronic health records (EHR), claims data, and predictive models to improve care quality and reduce readmissions. Cloud-based solutions are gaining traction due to scalability and cost efficiency, and there’s a growing emphasis on personalized risk profiles that include social determinants of health to provide equitable care. Adoption is also rising due to the demand for real-time dashboards and visual analytics that support operational and clinical strategy.
Segmentation: The Global Clinical Risk Grouping Solutions Market is segmented by Product (Scorecards & Visualization Tools, Dashboard Analytics Solutions, Risk Reporting Solutions, Software (Core Platforms) and Services), Deployment Model (Private Cloud, Public Cloud and Hybrid Cloud), Application (Population Health Management, Chronic Disease Management, Clinical Decision Support, Fraud Detection & Prevention and Other Specialized Applications), and Geography (North America, Europe, Asia-Pacific, Middle East and Africa, and South America). The report provides the value (in USD million) for the above segments.
Market Drivers:
Healthcare systems globally are shifting from volume-based to value-based care, emphasizing outcomes and cost efficiency. This transition increases demand for clinical risk grouping solutions that accurately stratify patient populations, enabling preventive interventions, optimized resource allocation, and improved chronic disease management.
In August 2025, the U.S. shift from fee-for-service to value-based care, driven by rising costs and inconsistent outcomes, boosted demand for clinical risk grouping solutions globally. As providers and payers emphasized preventive care, coordination, and outcome-based payments, tools for accurate risk stratification became essential. UnitedHealth Group’s leadership in value-based models further accelerated adoption, reinforcing the market’s growth and innovation. These platforms help measure performance against quality metrics and support pay-for-performance reimbursement, making them essential for hospitals and payers pursuing quality improvements. Integration with EHRs and advanced analytics further reinforces their role in enabling data-driven strategies, fostering widespread adoption across care settings.
Rapid advancements in artificial intelligence, machine learning, and big data analytics have significantly boosted the capabilities of clinical risk grouping solutions. AI-driven models enhance accuracy in risk stratification, reduce human error, and enable real-time insights from massive, heterogeneous datasets. These technologies empower providers to forecast patient outcomes, tailor interventions, and design personalized care plans more effectively. The integration of predictive analytics with EHRs, claims, and social determinants of health data expands the utility of risk solutions, driving market growth and innovation, particularly among larger healthcare systems and data-focused organizations.
Market Restraints:
A major restraint is the complexity of handling sensitive patient data across disparate systems while complying with stringent privacy regulations (e.g., HIPAA and GDPR). Integrating risk grouping tools with existing EHRs, claims platforms, and legacy systems requires significant technical infrastructure, skilled IT resources, and ongoing maintenance. High upfront implementation costs, especially for AI-rich solutions, pose barriers for smaller healthcare providers, particularly in emerging markets where budgets are constrained. These concerns, coupled with interoperability and standardization issues, slow adoption rates and complicate widespread deployment of clinical risk grouping solutions.
The clinical risk grouping solutions market significantly impacts healthcare systems and broader socioeconomic outcomes. By enabling precise identification of high-risk patients, these tools help reduce preventable hospitalizations, lower healthcare costs, and improve population health outcomes. Effective risk stratification supports value-based care, strengthening healthcare efficiency and enabling payers and providers to allocate resources more equitably. In emerging regions, adoption contributes to digital health expansion and workforce modernization. It also supports policy goals around chronic disease management and preventive care, ultimately reducing public health expenditures. However, ensuring equitable access across socioeconomic strata remains challenging due to implementation costs
Segmental Analysis:
The Dashboard Analytics Solutions segment is expected to witness the highest growth over the forecast period due to increasing demand for real-time, visual insights that enable faster clinical and administrative decision-making. Healthcare organizations are shifting toward data-driven care models, requiring intuitive dashboards to monitor patient risk scores, readmission rates, and population health trends. These solutions integrate multiple data sources, including EHR, claims, and lab data, to deliver actionable insights through customizable visualizations. As value-based care adoption rises, stakeholders need accessible dashboards to track quality metrics, financial performance, and operational efficiency. Consequently, dashboard analytics tools are becoming essential for risk stratification and care management.
The Public Cloud segment is expected to witness the highest growth over the forecast period due to its scalability, cost efficiency, and simplified deployment. Healthcare organizations increasingly prefer cloud-based risk grouping platforms that support remote access, seamless updates, and flexible storage for large datasets. Public cloud infrastructure enables fast integration with multiple data sources and offers better collaboration across care networks. Additionally, cloud providers offer strong security frameworks and compliance support, making public cloud adoption more attractive despite data sensitivity concerns. As hospitals and payers expand analytics capabilities, public cloud models provide a practical route to adopt advanced risk stratification tools without heavy upfront investment in IT infrastructure.
The Population Health Management segment is projected to record the highest growth as healthcare systems focus on preventive care and chronic disease management. Clinical risk grouping tools are integral to population health strategies because they identify high-risk groups and enable targeted interventions, improving outcomes while reducing costs. With rising chronic disease prevalence and an aging population, providers need scalable analytics solutions to monitor large patient cohorts and allocate resources efficiently. The shift toward value-based reimbursement further fuels demand, as payers and providers must demonstrate improved population outcomes. Population health management platforms increasingly incorporate social determinants of health and predictive modeling, strengthening their role in risk stratification and care coordination.
North America is expected to witness the highest growth over the forecast period due to advanced healthcare infrastructure, high digital health adoption, and strong emphasis on value-based care. The region has significant investment in healthcare IT, including EHR integration, analytics platforms, and AI-driven tools.
In May 2025, The merger of The Hardenbergh Group with Sentact and Preverity strengthened North America’s Clinical Risk Grouping Solutions Market by creating a unified, technology-driven leader in patient safety, clinical risk mitigation, and compliance. The combined platform enhanced data-driven risk management and oversight capabilities for major health systems, accelerating adoption of integrated risk solutions and driving competitive consolidation across the region.
Regulatory support and payer-driven reimbursement models encourage providers to adopt risk stratification solutions for better patient outcomes and cost control. Additionally, the presence of major market players and continuous innovation in predictive analytics accelerates market growth. High healthcare expenditure and rising demand for improved care quality further strengthen adoption rates, making North America the fastest-growing region in the clinical risk grouping solutions market.
The global market is highly competitive and moderately fragmented, featuring established healthcare IT companies, analytics providers, and specialized solution vendors. Firms compete through R&D, partnerships, mergers, and product enhancements to expand portfolios and geographic reach. Larger incumbents often integrate risk grouping into broader population health management suites, enhancing interoperability with EHR and clinical workflows. Strategic collaborations and acquisitions are common as companies seek to strengthen analytics capabilities and market share. Market competition is also fueled by emerging players focusing on niche offerings, such as AI-enhanced predictive platforms, tailored reporting tools, and cloud-native risk solutions.
The major players for above market are:
Recent Development
Q1. What are the main growth-driving factors for this market?
The market is driven by the global transition toward value-based care and the rising prevalence of chronic diseases. Healthcare payers and providers increasingly adopt these solutions to predict patient outcomes and manage costs. Furthermore, the integration of Big Data analytics and AI into population health management strategies significantly boosts market demand.
Q2. What are the main restraining factors for this market?
High implementation costs and a shortage of skilled IT professionals in healthcare limit market expansion. Data privacy concerns and the lack of interoperability between disparate EHR systems create significant barriers to seamless data integration. Additionally, resistance to changing traditional fee-for-service models in certain regions slows the adoption of risk-grouping technologies.
Q3. Which segment is expected to witness high growth?
The Public-cloud-based deployment segment is expected to witness the highest growth. Healthcare organizations are favoring cloud solutions due to their scalability, cost-effectiveness, and ability to facilitate real-time data access across multiple locations. This shift is particularly evident as remote monitoring and telehealth require flexible, accessible platforms for population health analysis.
Q4. Who are the top major players for this market?
Leading players include 3M Company (Health Information Systems), Optum (UnitedHealth Group), and Cerner Corporation. Other influential companies are Conduent, Inc., IBM Watson Health, and Nuance Communications. These organizations dominate by offering sophisticated algorithms that categorize patients based on clinical complexity, helping providers optimize resource allocation and improve clinical outcomes.
Q5. Which country is the largest player?
The United States remains the largest market for clinical risk grouping solutions. This dominance is attributed to a highly developed healthcare infrastructure, early adoption of digital health technologies, and strong regulatory mandates like the Affordable Care Act. The aggressive push toward risk-sharing models among American insurers continues to fuel regional growth.
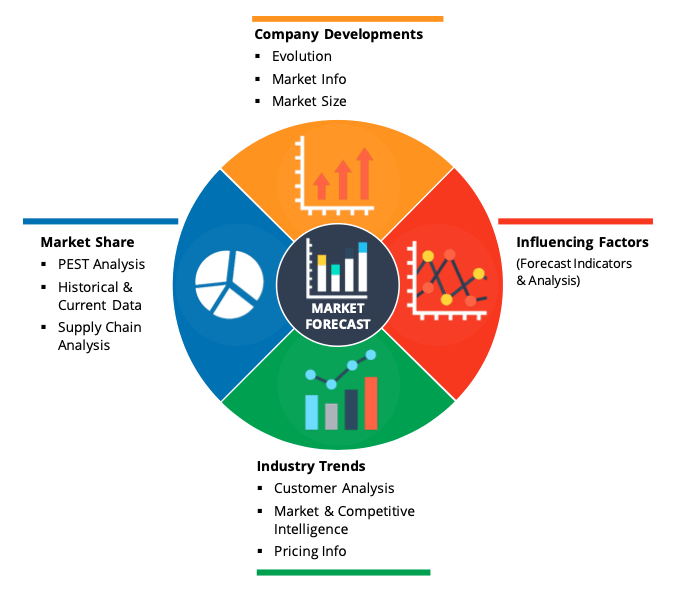
Data Library Research are conducted by industry experts who offer insight on industry structure, market segmentations technology assessment and competitive landscape (CL), and penetration, as well as on emerging trends. Their analysis is based on primary interviews (~ 80%) and secondary research (~ 20%) as well as years of professional expertise in their respective industries. Adding to this, by analysing historical trends and current market positions, our analysts predict where the market will be headed for the next five years. Furthermore, the varying trends of segment & categories geographically presented are also studied and the estimated based on the primary & secondary research.
In this particular report from the supply side Data Library Research has conducted primary surveys (interviews) with the key level executives (VP, CEO’s, Marketing Director, Business Development Manager and SOFT) of the companies that active & prominent as well as the midsized organization
FIGURE 1: DLR RESEARH PROCESS
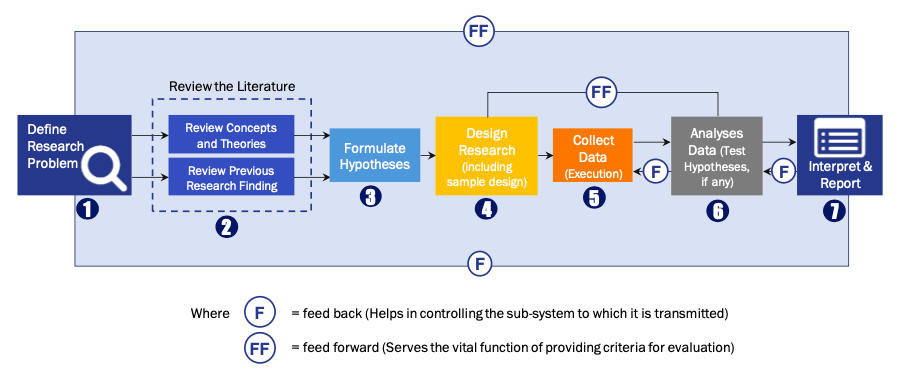
Extensive primary research was conducted to gain a deeper insight of the market and industry performance. The analysis is based on both primary and secondary research as well as years of professional expertise in the respective industries.
In addition to analysing current and historical trends, our analysts predict where the market is headed over the next five years.
It varies by segment for these categories geographically presented in the list of market tables. Speaking about this particular report we have conducted primary surveys (interviews) with the key level executives (VP, CEO’s, Marketing Director, Business Development Manager and many more) of the major players active in the market.
Secondary ResearchSecondary research was mainly used to collect and identify information useful for the extensive, technical, market-oriented, and Friend’s study of the Global Extra Neutral Alcohol. It was also used to obtain key information about major players, market classification and segmentation according to the industry trends, geographical markets, and developments related to the market and technology perspectives. For this study, analysts have gathered information from various credible sources, such as annual reports, sec filings, journals, white papers, SOFT presentations, and company web sites.
Market Size EstimationBoth, top-down and bottom-up approaches were used to estimate and validate the size of the Global market and to estimate the size of various other dependent submarkets in the overall Extra Neutral Alcohol. The key players in the market were identified through secondary research and their market contributions in the respective geographies were determined through primary and secondary research.
Forecast Model