The Global Healthcare Fraud Analytics Market is expected to grow at a compound annual growth rate of 24.3% from 2026 to 2033 to reach USD 16.23 billion by 2033, from USD 9.76 billion in 2026.
The Global Healthcare Fraud Analytics Market refers to the industry of software, platforms, and services designed to detect, prevent, and manage fraudulent activities within healthcare systems. Fraud analytics leverages big data, artificial intelligence (AI), machine learning (ML), and predictive modeling to analyze transactions, claims, and provider behavior to identify anomalies, waste, and abuse. These solutions help insurers, healthcare providers, and government payers safeguard revenue, reduce improper payments, and strengthen compliance with regulatory standards.
Key trends in the global healthcare fraud analytics market include increasing adoption of AI and machine learning to enhance anomaly detection accuracy and speed. Predictive analytics and natural language processing (NLP) are being integrated to interpret unstructured data from claims, clinical notes, and billing records. Cloud-based deployment and real-time analytics are gaining traction, enabling scalable, cost-effective solutions for payers and providers. Regulatory emphasis on reducing improper payments and rising healthcare costs has accelerated investment in fraud analytics. Partnerships between analytics vendors and healthcare stakeholders are expanding. Additionally, the emergence of network analytics and graph-based modeling is improving identification of complex fraud rings and behavioral patterns.
Segmentation: The Global Healthcare Fraud Analytics Market is segmented by Component (Solutions (Predictive Analytics, Machine Learning & AI Platforms, Data Visualization & Reporting Tools and Case Management Tools), and Services (Consulting, Integration & Support and Training & Education), Analysis Type (Real-time Analytics and Batch Analytics), Deployment Mode (Cloud-based and On-premises), Application (Claims Fraud Detection, Provider Fraud Analytics, Member/Beneficiary Fraud Detection, Prescription & Pharmacy Fraud Detection and Other Analytics (Billing, Identity, Network Abuse)), End User (Healthcare Payers (Insurance Companies), Healthcare Providers (Hospitals & Clinics), Government/Public Health Agencies, Pharmacy Benefit Managers (PBMs) and Others (Third-party Administrators, Employers)), and Geography (North America, Europe, Asia-Pacific, Middle East and Africa, and South America). The report provides the value (in USD million) for the above segments.
Market Drivers:
A primary driver of the healthcare fraud analytics market is the increasing prevalence of fraud, waste, and improper payments within healthcare systems globally. Complex billing schemes, duplicate claims, upcoding, and identity fraud result in substantial financial losses for insurers and government payers. As healthcare spending continues to rise, so does the incentive for fraudulent activity, prompting payers and providers to adopt robust analytics to detect and prevent losses.
Advanced fraud analytics tools leverage AI and predictive modeling to identify suspicious patterns that human auditors might miss. For instance, in June 2025, ICICI Lombard partnered with Clearspeed to deploy voice-based risk assessment technology, piloting it on motor theft claims to curb insurance fraud in India. The solution helped identify fraudulent claims more effectively, reflecting broader trends in fraud prevention. This reinforced the importance of analytics-driven fraud detection and increased demand for secure, scalable healthcare data storage systems to support large-scale fraud monitoring and compliance efforts globally. This escalating threat environment drives investments in automated, real-time fraud detection solutions to protect revenue and ensure compliance.
Regulatory pressure and stringent compliance requirements are significant drivers of the healthcare fraud analytics market. Governments and oversight bodies worldwide are imposing stricter standards to reduce healthcare fraud, waste, and abuse, particularly in public insurance programs like Medicare and Medicaid. Regulations mandate robust monitoring and reporting systems to detect anomalies and improper payments. Failure to comply can result in penalties, financial losses, and reputational damage for payers and providers. As a result, healthcare organizations are investing in analytics platforms to meet regulatory expectations and demonstrate accountability. Fraud analytics enhances audit readiness, supports regulatory reporting, and fosters transparency, driving broader technology adoption across the sector.
Market Restraints:
A key restraint for the global healthcare fraud analytics market is the complexity and cost associated with implementation and integration. Deploying advanced analytics solutions often requires significant upfront investment in software licenses, infrastructure, and skilled personnel. Integration with existing claims processing systems, electronic health records (EHR), and payer databases can be technically challenging and time-consuming. Smaller insurers and healthcare organizations may lack the financial resources or IT expertise needed for seamless integration and long-term maintenance. Additionally, data quality and interoperability issues can hinder analytics effectiveness. These barriers slow adoption, particularly among resource-limited entities, delaying the full realization of fraud detection benefits.
The healthcare fraud analytics market has a significant socioeconomic impact by reducing financial losses due to fraud, waste, and abuse, thereby lowering healthcare costs for payers and patients. Fraudulent claims and billing errors strain public insurance programs and increase premiums for private policyholders. By detecting and preventing improper payments, analytics solutions free up resources for patient care, preventive services, and innovation. Enhanced fraud detection also supports healthcare system sustainability and public trust. Moreover, reduced administrative burden improves operational efficiency for insurers and providers. However, widespread adoption requires investment in technology and skilled personnel, which may challenge smaller organizations without sufficient resources.
Segmental Analysis:
The integration and support segment is expected to witness the highest growth over the forecast period as healthcare organizations increasingly seek end-to-end fraud analytics implementation. Advanced fraud detection systems require seamless integration with existing claims processing, EHR, billing, and provider databases. Integration services ensure data quality, interoperability, and real-time processing, while ongoing support helps maintain system performance, update models, and manage regulatory changes. Many organizations lack in-house expertise to deploy complex analytics solutions, driving demand for third-party integration and managed services. Additionally, rising adoption of AI-based fraud analytics increases the need for continuous tuning, validation, and user training, further fueling growth in this segment.
The cloud-based segment is expected to witness the highest growth over the forecast period due to its scalability, cost efficiency, and faster deployment. Cloud fraud analytics solutions enable healthcare payers and providers to process large volumes of claims data without heavy upfront infrastructure investment. Cloud platforms also support real-time analytics, automated updates, and easier collaboration across multiple sites. The growing shift toward digital transformation and remote operations has accelerated cloud adoption, allowing organizations to access advanced AI and machine learning tools without managing complex IT systems. Additionally, cloud-based solutions offer improved disaster recovery, data backup, and flexibility, making them increasingly attractive for healthcare organizations seeking modern fraud detection capabilities.
The claims fraud detection segment is expected to witness the highest growth over the forecast period as fraudulent claims continue to represent a major cost burden for payers and government programs. Claims processing generates vast amounts of data, making it a key target for analytics-driven fraud detection. Advanced AI and machine learning models can identify anomalies such as duplicate claims, upcoding, and suspicious billing patterns with higher accuracy and speed than manual audits. Increasing regulatory scrutiny and rising healthcare costs have pushed insurers to invest in automated claims analytics to reduce improper payments and improve operational efficiency. As claims fraud remains prevalent, demand for robust detection solutions is expected to grow significantly.
The healthcare payers segment is expected to witness the highest growth over the forecast period due to the critical need to control fraud-related losses and improper payments. Insurance companies process millions of claims annually, making them highly vulnerable to fraud, waste, and abuse. Fraud analytics platforms enable payers to detect suspicious patterns, flag high-risk providers, and prevent fraudulent claims before payments are issued. With rising healthcare costs and tighter regulatory scrutiny, payers are investing heavily in AI-based analytics to improve accuracy and reduce manual review workloads. Additionally, payers are increasingly partnering with technology vendors to enhance real-time monitoring and strengthen compliance, driving significant market growth in this segment.
North America is expected to witness the highest growth in the global healthcare fraud analytics market over the forecast period due to high healthcare spending and strong regulatory focus on fraud prevention.
The region’s large and complex insurance market, including Medicare and Medicaid programs, creates significant exposure to fraudulent claims and improper payments. For instance, in January 2025, The U.S. filed a False Claims Act complaint against Priority Hospital Group and affiliated LTCHs for allegedly providing medically unnecessary care and delaying discharges to increase Medicare reimbursements, violating the Anti-Kickback Statute and Stark Law. This highlighted persistent healthcare fraud and improper payments, reinforcing the need for advanced fraud detection and secure data storage solutions, thereby strengthening demand in North America’s healthcare data storage market.
Government initiatives and stringent compliance requirements have accelerated adoption of advanced analytics solutions among payers and providers. North American healthcare organizations also have robust IT infrastructure and higher digital maturity, enabling faster deployment of AI-driven fraud detection systems. Additionally, ongoing investments in big data, cloud computing, and machine learning technologies support continued growth of fraud analytics across the region.
The competitive landscape of the global healthcare fraud analytics market is shaped by established technology firms, specialized analytics vendors, and emerging AI innovators. Key players differentiate through advanced machine learning models, real-time processing capabilities, and domain expertise in healthcare claims and provider behavior. Strategic partnerships with insurers, health systems, and government agencies strengthen market position. Vendors compete on accuracy, scalability, integration with existing claims processing systems, and ease of deployment (on-premises vs. cloud). Ongoing innovation in predictive modeling, NLP, and network analysis intensifies competition. Mergers and acquisitions are common as larger firms expand analytics portfolios, while smaller specialists focus on niche solutions and customizable offerings.
The major players for above market are:
Recent Development
Q1. What are the main growth-driving factors for this market?
The market is primarily driven by the increasing number of fraudulent healthcare claims and rising medical identity theft. The surge in healthcare spending, coupled with the transition toward electronic health records, necessitates advanced prepay detection systems. Additionally, government mandates to curb rising insurance premiums and operational losses are fueling the adoption.
Q2. What are the main restraining factors for this market?
Growth is hampered by the high initial investment required for deploying sophisticated analytics platforms and a lack of skilled professionals to manage them. Concerns over data security and the complexity of integrating new software with legacy healthcare systems also pose challenges. Furthermore, many organizations remain hesitant due to unclear return-on-investment timelines.
Q3. Which segment is expected to witness high growth?
The predictive analytics segment is expected to witness the highest growth. Unlike traditional descriptive tools, predictive modeling uses machine learning to identify suspicious patterns before claims are paid. This shift from "pay-and-chase" to "prevent-and-protect" strategies is highly valued by insurance payers looking to minimize financial leakage and improve operational efficiency.
Q4. Who are the top major players for this market ?
The market is led by prominent technology and healthcare firms including IBM Corporation, Optum (UnitedHealth Group), SAS Institute, and Oracle. Other significant players include LexisNexis Risk Solutions, Conduent, and Cotiviti. These companies dominate by offering integrated cloud-based platforms that combine behavioral analytics with massive databases to flag anomalies in real-time.
Q5. Which country is the largest player?
The United States is the largest player in the healthcare fraud analytics market. This is due to a highly developed healthcare infrastructure, a high volume of insurance claims, and stringent regulations like the False Claims Act. The presence of major industry players and significant investments in digital health further solidify its position.
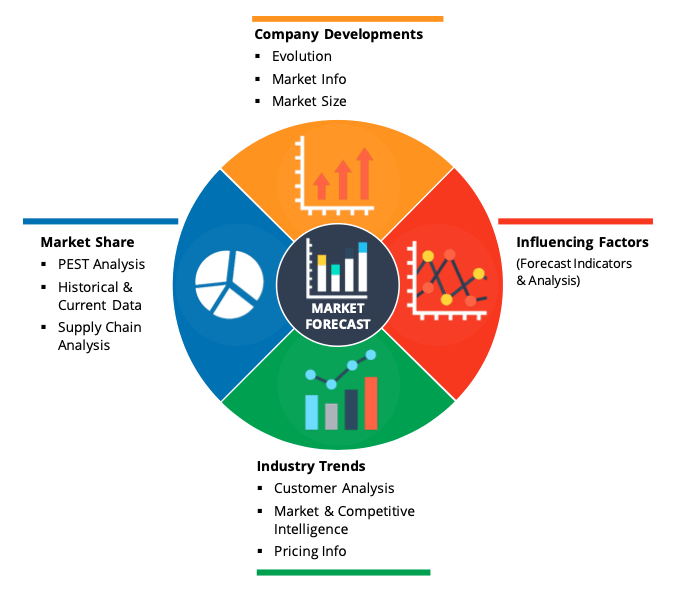
Data Library Research are conducted by industry experts who offer insight on industry structure, market segmentations technology assessment and competitive landscape (CL), and penetration, as well as on emerging trends. Their analysis is based on primary interviews (~ 80%) and secondary research (~ 20%) as well as years of professional expertise in their respective industries. Adding to this, by analysing historical trends and current market positions, our analysts predict where the market will be headed for the next five years. Furthermore, the varying trends of segment & categories geographically presented are also studied and the estimated based on the primary & secondary research.
In this particular report from the supply side Data Library Research has conducted primary surveys (interviews) with the key level executives (VP, CEO’s, Marketing Director, Business Development Manager and SOFT) of the companies that active & prominent as well as the midsized organization
FIGURE 1: DLR RESEARH PROCESS
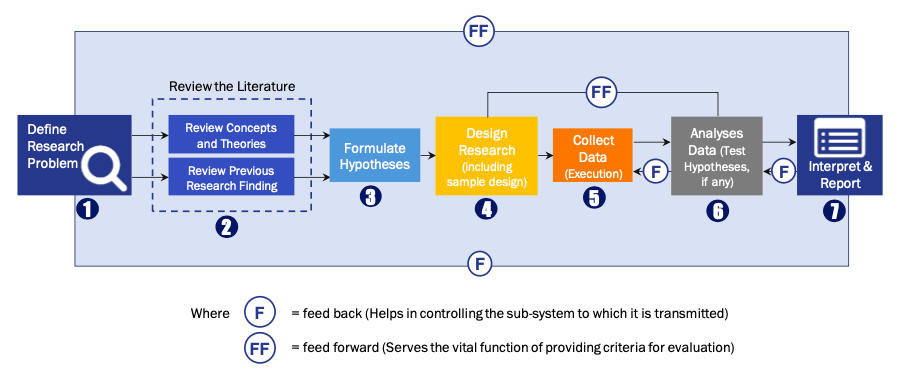
Extensive primary research was conducted to gain a deeper insight of the market and industry performance. The analysis is based on both primary and secondary research as well as years of professional expertise in the respective industries.
In addition to analysing current and historical trends, our analysts predict where the market is headed over the next five years.
It varies by segment for these categories geographically presented in the list of market tables. Speaking about this particular report we have conducted primary surveys (interviews) with the key level executives (VP, CEO’s, Marketing Director, Business Development Manager and many more) of the major players active in the market.
Secondary ResearchSecondary research was mainly used to collect and identify information useful for the extensive, technical, market-oriented, and Friend’s study of the Global Extra Neutral Alcohol. It was also used to obtain key information about major players, market classification and segmentation according to the industry trends, geographical markets, and developments related to the market and technology perspectives. For this study, analysts have gathered information from various credible sources, such as annual reports, sec filings, journals, white papers, SOFT presentations, and company web sites.
Market Size EstimationBoth, top-down and bottom-up approaches were used to estimate and validate the size of the Global market and to estimate the size of various other dependent submarkets in the overall Extra Neutral Alcohol. The key players in the market were identified through secondary research and their market contributions in the respective geographies were determined through primary and secondary research.
Forecast Model